Rehab for Kevin Durant Knee Injury: Grade II MCL Sprain
Golden State Warriors superstar Kevin Durant sustained a knee injury recently and the concern was that he tore the dreaded ACL. Fortunately for him, his team, and his fans, he just has an MCL or medial collateral ligament injury. He’ll be out about a month or so. A general “athletic training room rule” for MCL injuries is about 2 weeks out for each grade of strain. He’s got a Grade II according to reports, so that is about right. So what’s with the MCL and why will Kevin Durant be out a month?


What’s the MCL?
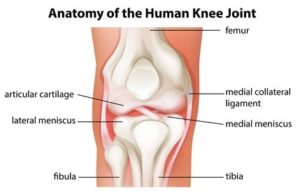
The MCL is a ligament along the medial aspect of the knee. It’s more of a thickening of the joint capsule, more “sheet-like.” It is also an extra-articular ligament, or outside the joint. On the contrary, the infamous anterior cruciate ligament (ACL) is intra-articular, or inside the knee and is more “rope-like.” There are four knee ligaments that contribute to knee stability, and the MCL helps prevent the knee from “buckling” to the inside. Here is a comprehensive link on MCL anatomy and function.
How is it injured?
Most of the time, the MCL is injured from a blow to the outside or lateral aspect of the knee which causes the knee to buckle inward. However, the MCL can also be torn from an awkward cut or land from a jump, which is something Kevin Durant does constantly in basketball. It can be injured in the mid-substance over the joint line, or off of its bony attachments on the tibia or the femur.


Cutting, crossovers, and change of direction happen regularly in basketball and leave players at risk for MCL injury
How long do they usually take to heal?
In pro sports, medical staffs must have the clearest crystal ball of any other professional. Before the injury is accurately diagnosed, a host of stakeholders have to know how long they’ll be out- coach, general manager, agents, etc. A general rule in sports medicine with MCL injuries is that it is about two weeks of time loss for each grade of tear. Therefore, with a Grade I tear, expect two weeks out, Grade II four weeks, Grade III tear would be approximately 6 weeks out. Certainly, this rule is not an absolute as athletes may require more or less time. Proximal, or femoral attachment MCL sprains, tend to heal a little faster but can stiffen up. On the contrary, distal or tibial attachment tears tend to heal slower, but typically aren’t as stiff. All that said, injury history, concomitant injuries, time of season, level of play, and athlete confidence are just a few of several other considerations that affect return to play.
Why is an MCL sprain a big deal?
As a professional basketball player, Kevin Durant is frequently cutting and changing direction as well as jumping and landing on that knee. Given that the MCL provides medial stability to the knee and helps prevent “buckling” of the knee, it’s critical for him that this ligament is doing its job. Not only is it painful, but without proper healing, the ligament can not only heal in a lengthened state but will also have poor quality tissue in the healing process (think straight lines which are preferred, versus criss-crossing fibers). You don’t want the ligament to continue the cycle of healing and re-injury. The ligament will be weaker and heal in an elongated state, thereby making it insufficient. So if Kevin Durant doesn’t do this right, this could haunt him for a long time.
Physical Therapy for MCL Sprains
The rehab for MCL sprains depends of course on severity of the sprain. The more serious the sprain, the slower the process. With an acute, severe sprain, the athlete is likely to need crutches, a brace, and graded range of motion progression. Progressing range of motion too fast with this injury may cause more pain and impede optimal healing of the ligament. In general though, here’s a rehab outline:
- Control pain.Icing, compressive wrapping, a knee brace, and use of a crutch or crutches will all help reduce pain and promote healing of the ligament. Another “training room trick” is to put a medial heel wedge in the shoe of the affected knee. Effectively, the medial wedge decreases strain on the healing ligament by compressing the medial joint line, even if only a little. It’s one of those interventions that is by no means a game-changer, but can help.
- Low-intensity pulsed ultrasound (LIPUS).There was a time when ultrasound was used for everything. Therefore, its effectiveness has continually been debated and questioned. Unfortunately, it has been discarded as a useful modality and this is actually one injury where it may help. However, there are some good studies supporting the use of LIPUS for MCL healing here, here, and here Laser therapy is also an option and can be effective for these capsular ligaments near the surface.
- Restore range of motion.The use of a bike, pool, or heel slides are all ways that can help an athlete restore their range. The optimum stimulus for regeneration of ligaments is modified tension in the line of stress, and tons of repetitions at that. That is precisely why cycling is a great modality for these injuries. With more severe sprains, a graded range of motion progression may be done to help prevent over-straining of weakened, painful tissue. Therefore, an athlete may have 30-90° for a couple of days, then open 10° in each direction every day or two after until full range is restored. In more chronic cases with pain in specific ranges of motion, instrument assisted soft tissue mobilization can help break up scar tissue and facilitate healing. There is one study using these instruments for this injury from the Journal of Orthopedic and Sports Physical Therapy that supports use of these tools to facilitate healing. Just because of pain, it is not recommended to use the instruments acutely. They’re best suited for chronic injuries/chronic phases of healing.
- Strengthening of the lower extremity. All sagittal movements (moving forward) should be painless prior to initiation of lateral and rotational movements. Lunges, step ups, squats, and leg press are just a few exercises that can be utilized. Of course, strengthening the hips should be a part of a comprehensive program for this injury. One word of caution – hamstring curls can be painful with this injury. Proceed carefully. Once straight-ahead movements are tolerated, progressing to lateral and rotational movements should follow.
- Graded progression of return to sports activities. Forward jogging can commence once range of motion is restored and the athlete has passed strength testing. Speed will be gradually increased. 45° cuts, shuffling, and 90° cuts would follow, then the athlete would progress to more field-based sport-specific drills. For soccer, this injury can be particularly challenging because of kicking, especially with the “push” kick/pass. The rotation of the lower leg can stretch the MCL and cause pain. A good progression is non-contact individual drills non-contact team drills, contact drills, then full release to activities.
Once sports activities are painless and the athlete’s confidence is restored, return to play should be considered. Regarding bracing with these injuries, it’s really a personal preference of the athlete. Offensive/defensive linemen might consider wearing it due to bodies crashing into each other and lots of lateral, contact movements. Unfortunately, these braces sometimes make athletes a target for insidious actions by opponents.
No question, this could have been a much worse injury for Kevin Durant. He got away with one evidently. We’re sure he’ll recover from this and be back to his normal self again.
It would be a privilege to serve you and partner with you in your care if you have an MCL injury. (913) 728-8599 We have locations in Overland Park and Prairie Village to serve you.
Tags: Kansas City, Kevin Durant, Kevin Durant injury, Kevin Durant rehab, Overland Park, Physical Therapy, prairie village, sports physical therapist